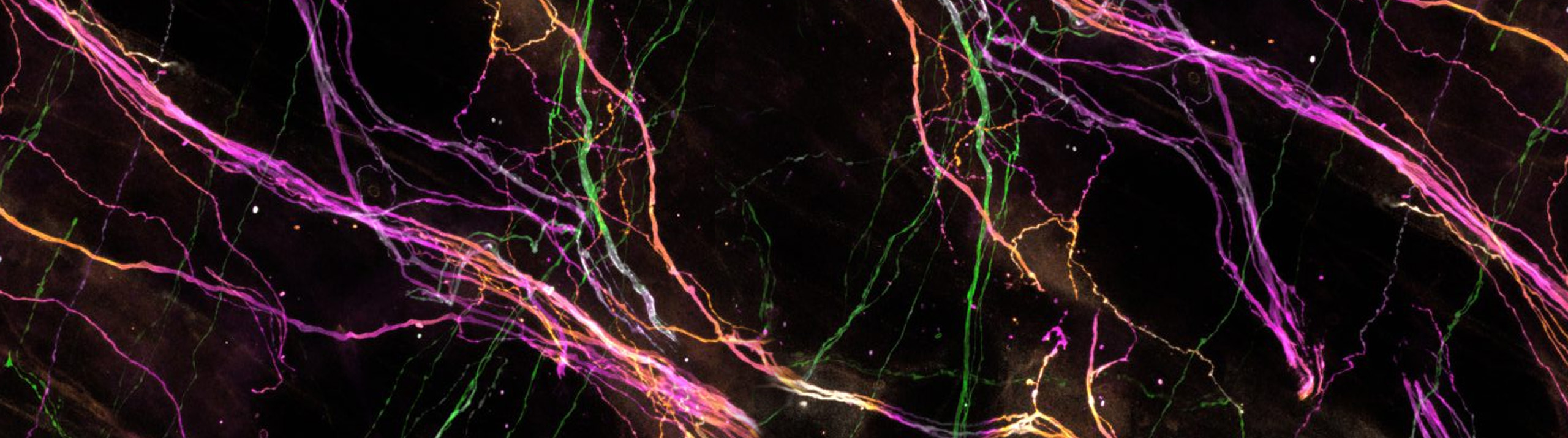
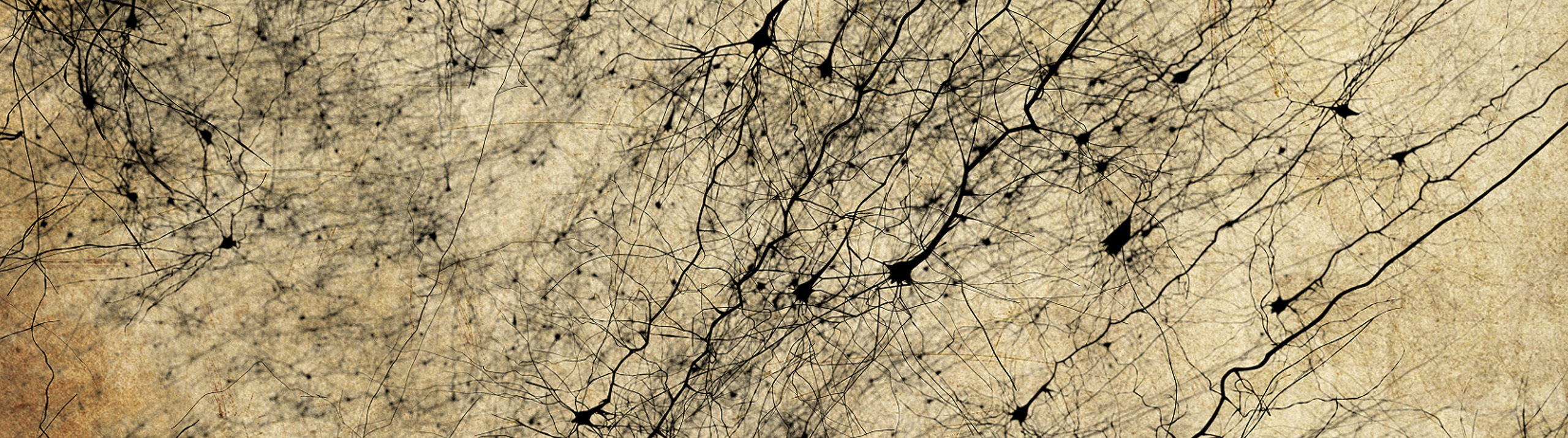
Researchers at Colorado College may have identified a new neuropathological hallmark of Chronic Traumatic Encephalopathy (CTE). Their findings, published in the Journal of Comparative Neurology, describe overall dendritic atrophy across cortical neurons and greater morphological variability in CTE brains compared to controls. A neurodegenerative disorder characterized by late-onset symptoms like depression, confusion, and memory loss, CTE is caused by repeated impacts to the brain. The disease...
Read MoreAlzheimer’s Disease
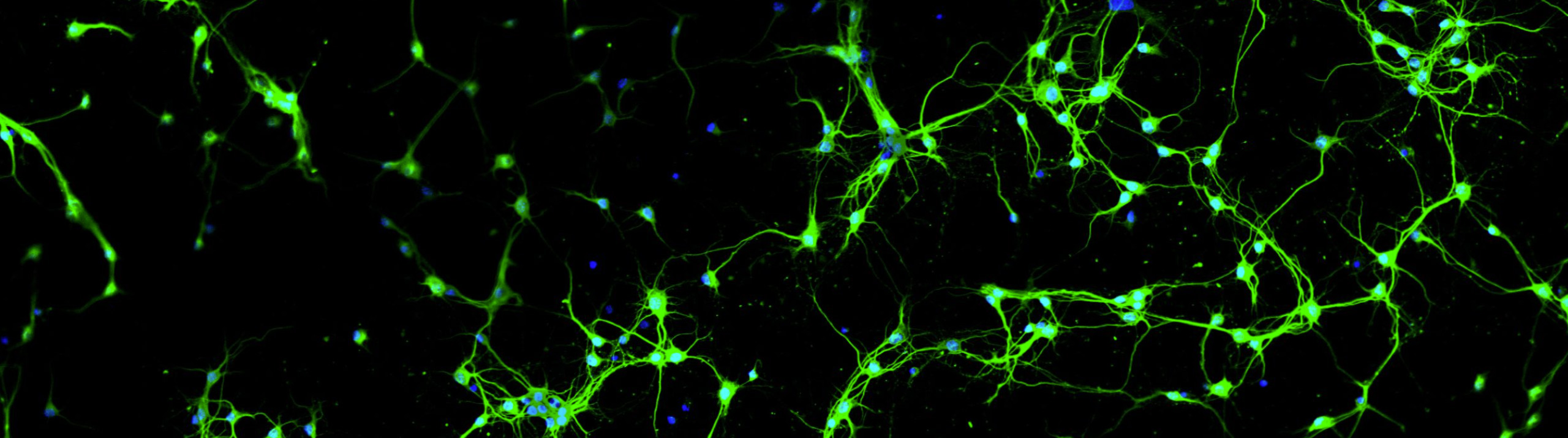
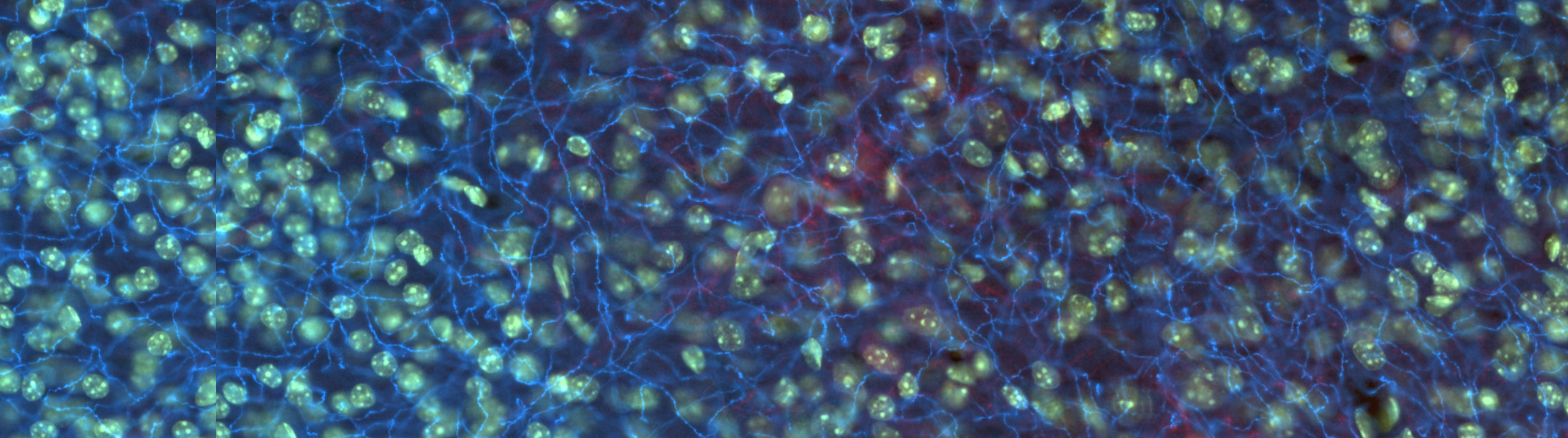
Scientists at Western Sydney University used Stereo Investigator and Neurolucida 360 to quantify cells in a mouse model of neuroinflammation after feeding mice two different curcumin formulations. Some inflammation is normal in a healthy mammalian brain. But as the brain ages, processes can break down, leading to chronic neuroinflammation. This can develop into Alzheimer’s disease, dementia, and other neurodegenerative diseases. Scientists at Prof. Gerald Muench’s lab, at...
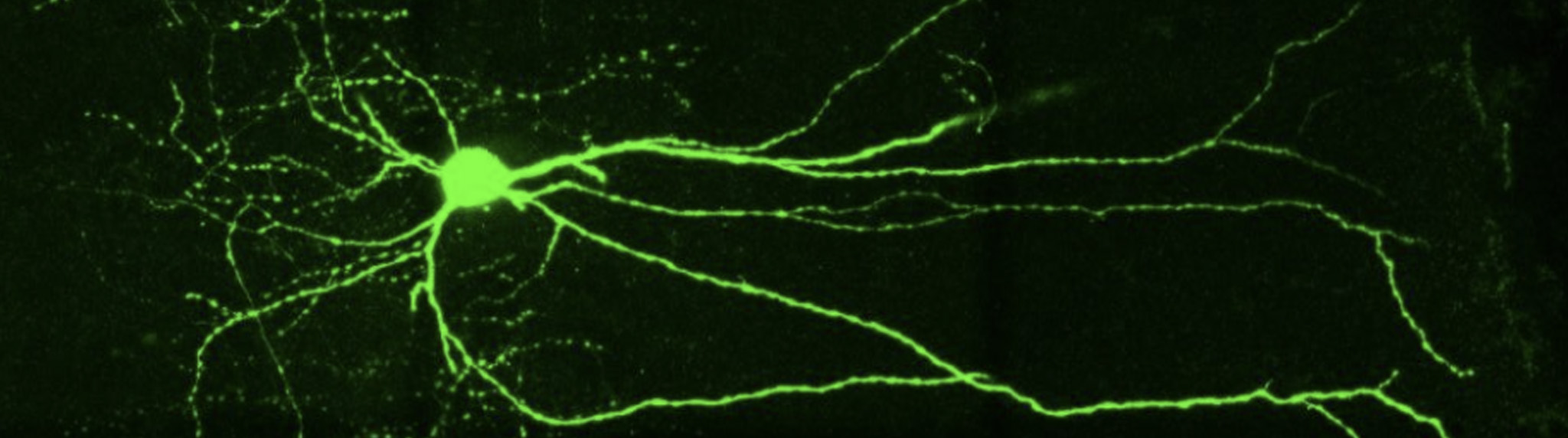
Read MoreNeurolucida 360 Used to Analyze Dendrites and Dendritic Spines Amyloid plaques and tau tangles are the hallmarks of Alzheimer’s disease (AD) pathology, but synapse loss is what causes cognitive decline, scientists say. In a paper published in Science Signaling, researchers at the Herskowitz Lab, at the University of Alabama at Birmingham, used Neurolucida 360 to analyze spine density and dendritic length in hAPP mice — a...
Read MoreAstrocytes (GFAP) in the dentate gyrus of a mouse hippocampus. Image courtesy of Dr. Ahmad Salehi, Stanford University. It is well known that physical exercise eases the symptoms of neurodegenerative disorders like Alzheimer’s disease and helps to prevent their onset. Researchers at Stanford University are working on figuring out how it happens. In their study, published in the journal Brain Structure and Function, scientists in Dr....
Read More[caption id="attachment_6094" align="alignright" width="231"] Micrograph of cholinergic neurons in the nucleus basalis of Meynert. Image from Wikipedia.[/caption] Cholinergic neurons degenerate at devastating rates in Alzheimer's disease, but Dr. Mark Tuszynski and his team at the University of California, San Diego may have found a way to slow the decline. Their study, published in JAMA Neurology, reports that nerve growth factor gene therapy increased the size, axonal sprouting, and signaling of cholinergic neurons...
Read MoreNeurolucida Helps Scientists Discover that Gorillas are Relevant in the Study of Alzheimer’s Disease
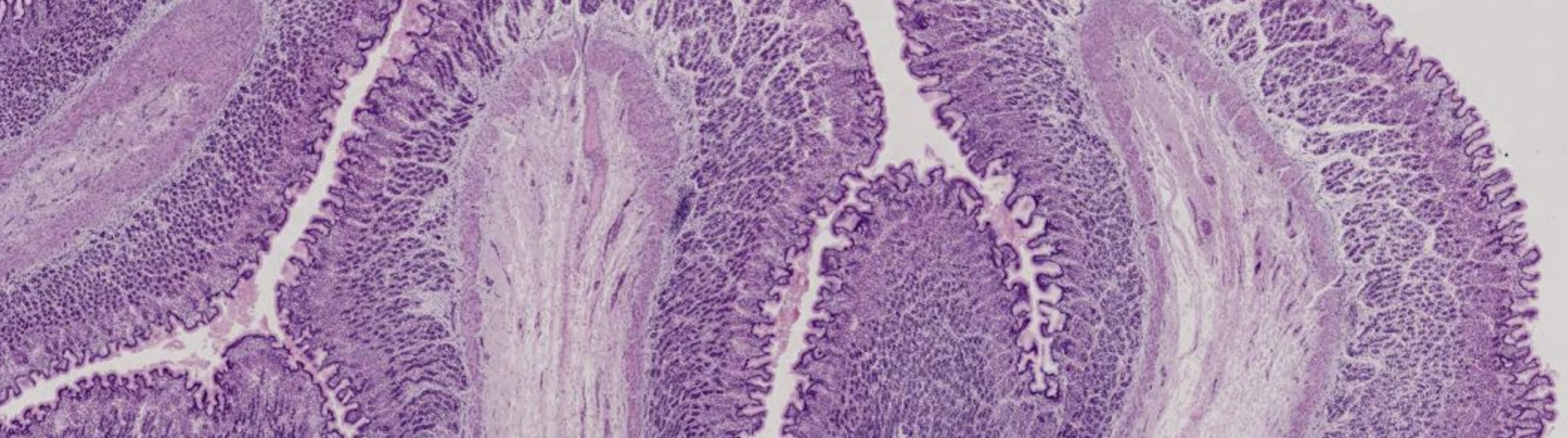
Humans and gorillas are approximately 98% identical on a genetic level, however there is little published research exploring Alzheimer's disease pathology in gorillas. A new paper reports that gorillas display similarities in advanced age to humans ̶ including the presence of Alzheimer's disease precursors like amyloid-beta (Aβ) plaques and tau lesions. The study, published in the Journal of Comparative Neurology, provides evidence of Alzheimer's disease precursors in the western...
Read MoreNeurotrophic factors may be the key to the cure for Parkinson’s, Huntington's, Alzheimer's, and other neurodegenerative disorders. Scientists have known this for over twenty years. But the question continues to loom – how does one safely and effectively deliver the neurotrophic factors to the damaged neurons? Dr. Raymond Bartus and his team at Ceregene, a biotechnology company in San Diego, have developed an innovative approach...
Read MoreAlzheimer's disease is the most common form of dementia. Most cases occur in people over 65, and are not genetically inherited. Roughly five percent of Alzheimer's patients suffer from familial Alzheimer's disease (FAD), an uncommon form that tends to strike sooner, and is related to a genetic predisposition - most commonly, a mutation in the presenilin 1 gene (PS1). A recent study, led by Dr. Miguel...
Read More